TEECOM Welcomes Jordan Rivchun as Principal, Vice President Client Relations
TEECOM is proud to announce the hiring of Jordan Rivchun as Principal, Vice President...
The simple nurse call bell has transformed from a basic alarm system into a critical piece of technology in every patient room, acting as an intelligent hub for data, communication, workflow, and safety. Our healthcare team recently toured the facilities of multiple nurse call manufacturers to learn about how this technology continues to advance and improve staff efficiency and patient satisfaction. We gathered their insight and have highlighted takeaways on how nurse call systems are impacting patients, staff, and the built environment.
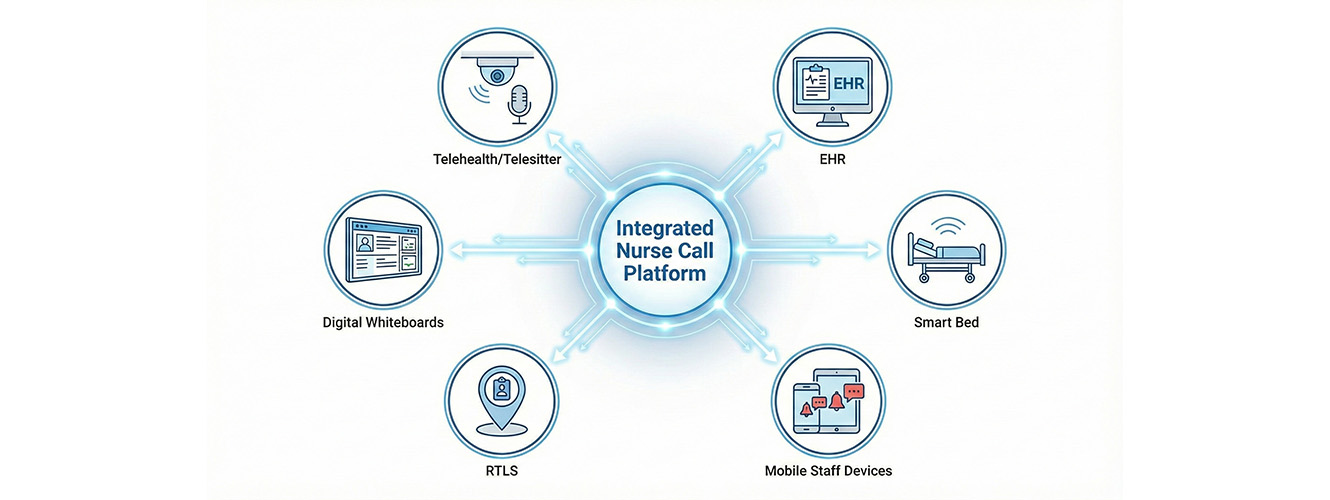
A significant feature of modern nurse call systems is the seamless integration of telehealth and telesitter functions. Instead of operating three separate systems—one for nurse call, one for virtual visits, and one for remote patient observation—manufacturers are now integrating in-room components (such as a ceiling mic and a camera). This ability to integrate virtual nursing, telesitting, and even virtual family visits with the nurse call system is a significant benefit for reducing hospitals’ technology budgets. Additionally, integrating with the Electronic Health Record (EHR) ensures simplicity and efficiency, streamlining provider workflows and providing a more seamless patient experience.
When hospitals discuss their wish lists for new nurse call systems, it typically comes down to two primary factors: cost and efficiency.
The modern nurse call is becoming the ultimate connection point, linking up with almost every other system in the hospital to create a cohesive patient environment.
The new capabilities are directly improving the patient’s stay, making them feel safer, more informed, and more comfortable. The system is acting as the central controller for the patient environment. For instance, an in-room control device, commonly a tablet, is not only connected to the nurse call system but also integrates with other aspects of the patient room, allowing patients to control aspects like room temperature, lighting, shades, and entertainment directly.
Beyond controls, the system integrates heavily with patient education (showing informational videos from providers such as WebMD), entertainment (connecting to streaming services like Netflix and Hulu), and even food ordering. To make it easier, many facilities now offer a Bring Your Own Device (BYOD) option, where a room-specific QR code directs patients to a link to download a helpful app.
On the safety front, location technology via RTLS not only streamlines staff response but also boosts patient confidence by providing accurate timestamping for staff arrival. As mentioned earlier, the interface with the patient’s smart bed is helpful for fall prevention, utilizing simple visual and verbal cues to keep them safe.
While the advancements in patient room technologies are exciting, implementing these complex, data-heavy systems isn’t without its challenges.
The future of nurse call is all about network connectivity, data, and simplified deployment. We anticipate a significant shift away from older, centralized nurse call hardware and towards fully network-based, IP-connected systems that meet all code requirements. The following are some examples of where we see nurse call technology heading.
Ultimately, increasing the number of IP connections across the system will unlock the potential for advanced features and functionality we are only just beginning to imagine. The continued integration of nurse call systems into a hospital’s technology ecosystem can provide significant benefits by increasing workforce efficiency and patient satisfaction scores. However, even though the possibilities may be endless, choosing the right solution for your facility will require careful technology visioning.
Engaging a technology consultant, like TEECOM, helps alleviate the burden of coordination within the design team. Our healthcare team utilizes their decades of experience to translate owner technology needs, to practical design strategies that create efficient buildings, staff workflow, and patient experiences. Will any of these advancements impact your next facility? Visit our contact page to get in touch with one of our healthcare experts and dive deeper into how you can build your hospital FOR the future.
Nikki Tuft is a telecom designer with over 25 years of experience in systems design, layout, value engineering, and project management with multiple healthcare technology systems. Over the years, she’s had the opportunity to lead projects ranging from 5,000 sf to over 1,000,000 sf, assisting clients with implementing their vision to meet project goals and expectations.
Bryan Herrin is an expert in nurse call system design. He brings over 30 years of experience designing and delivering low-voltage technology systems that enhance safety, efficiency, and performance in complex environments. He has focused extensively on healthcare, specializing in nurse call, access control, video surveillance, RTLS, and public address systems. Known for his practical insight and years of hands-on experience, Bryan is skilled at guiding projects from initial design to successful completion.
Stay ahead of the curve with our latest blog posts on industry trends, thought leadership, employee stories, and expert insights.